Psych Hpi Template
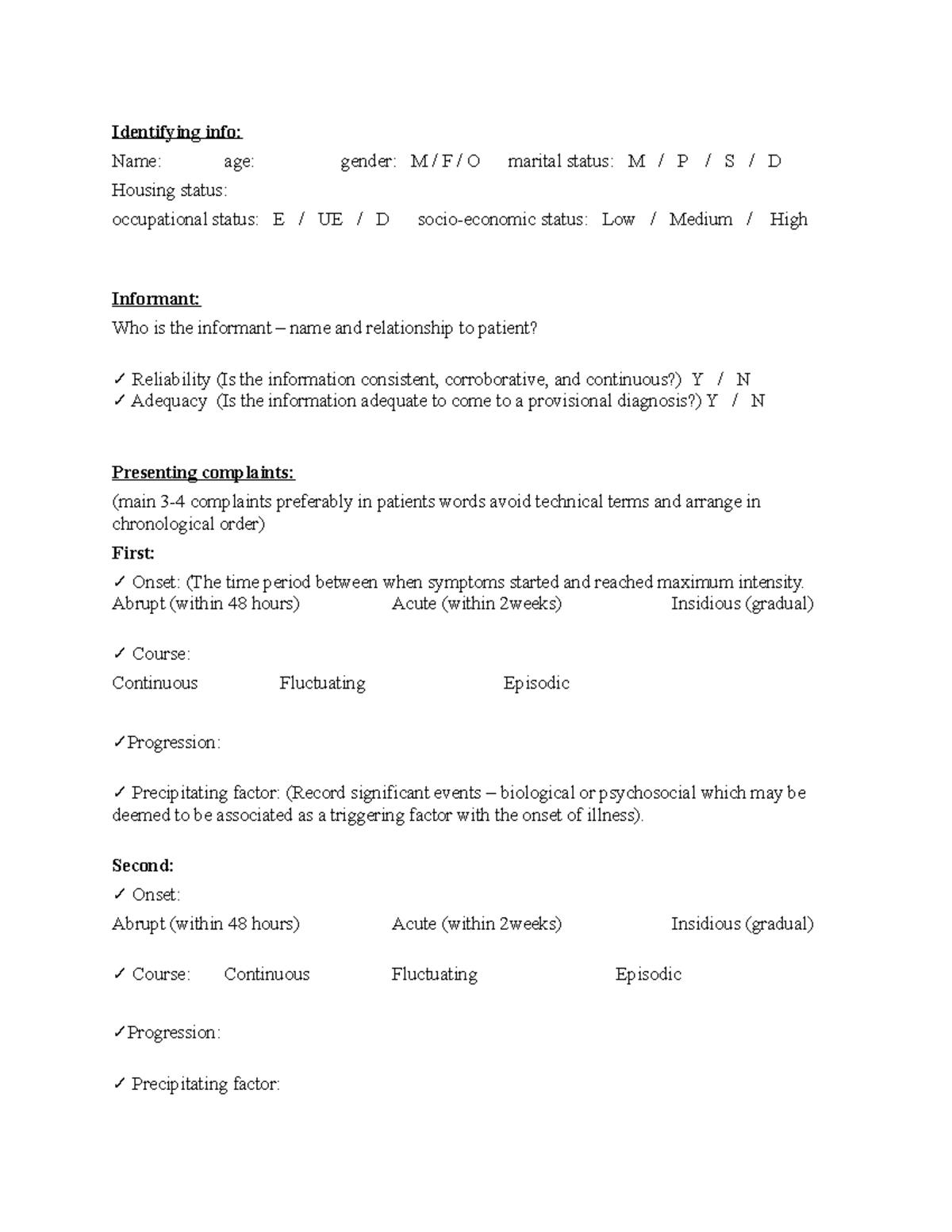
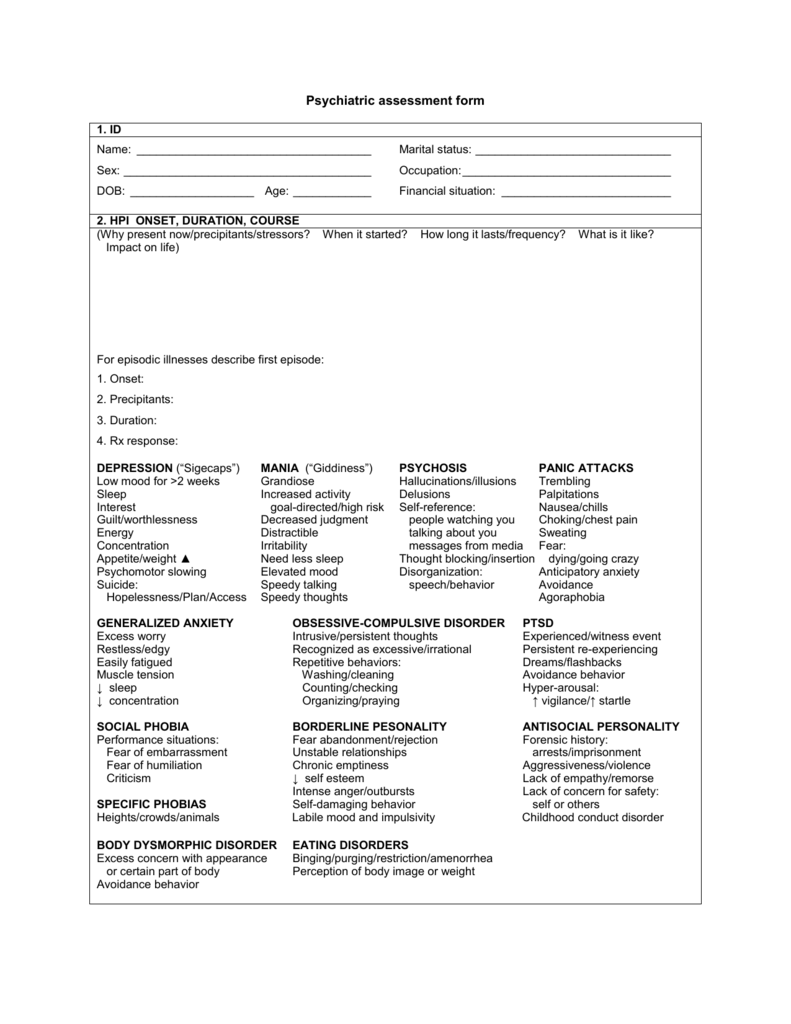
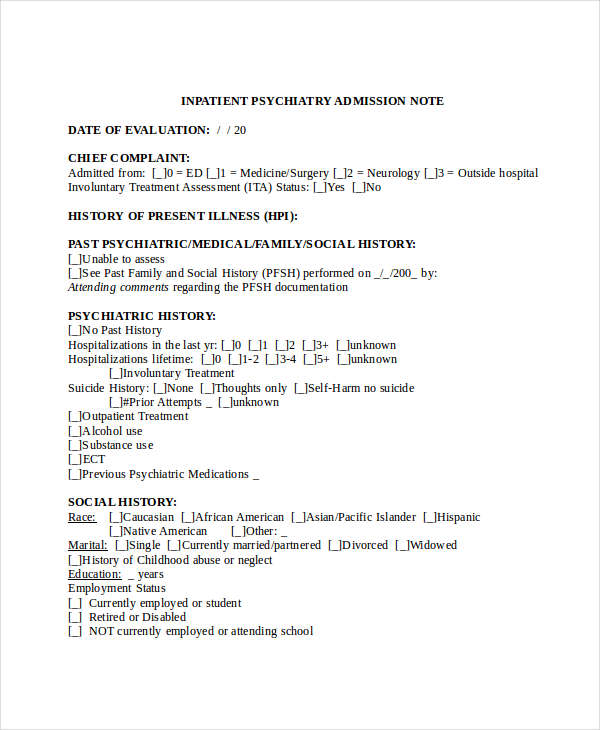
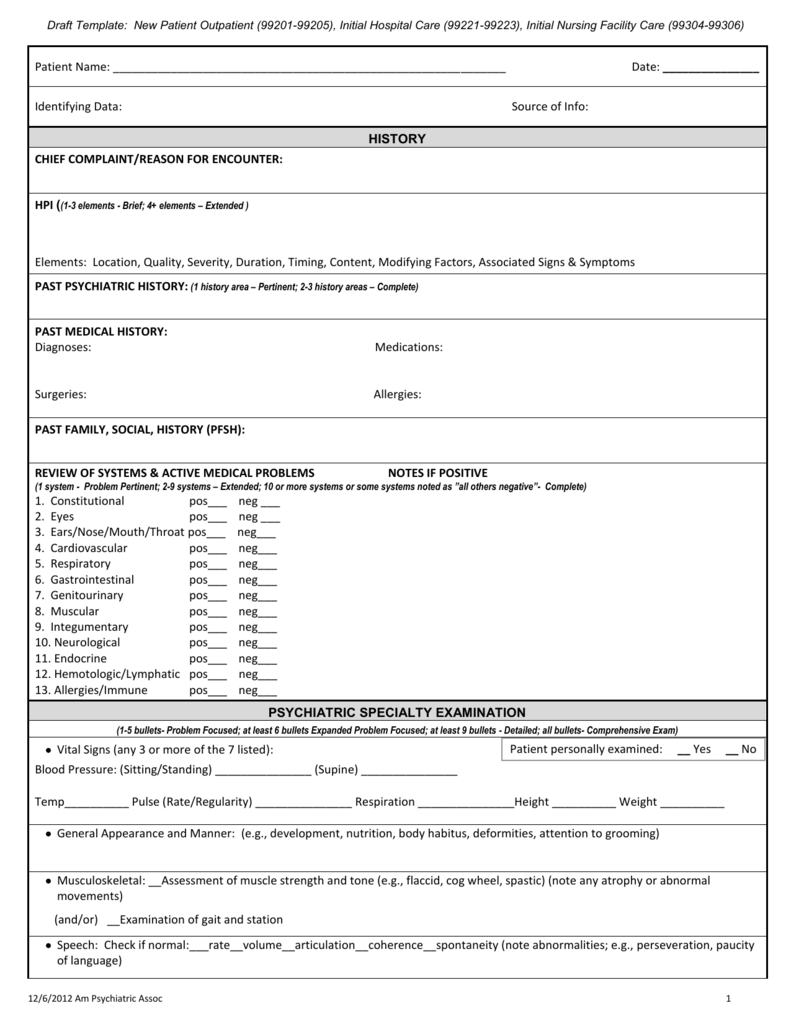
Psych Hpi Template - Quality, severity, duration, timing, context, modifying factors, associated signs and symptoms): Ideally, this should be in the patient’s words. This is a template that. Trying to see what the best intake guide or sheet you've had or utilized to interview a patient during your psychiatry rotation. As a mental health practitioner, you will come across a myriad of diverse documentation templates in the course of your professional endeavors: The history of present illness (hpi) component of an e/m service is comprised of eight elements: There are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. (document at least 4 of the following elements of the present illness: The template provides guidance on what to include in each section, such as ensuring a thorough medical review of systems, asking about family psychiatric history, and including discharge. In this blog, we aim at mentalyc to describe the standard components of the mental status examination process while offering suggestions for carrying it out respectfully and insightfully. There are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. (document at least 4 of the following elements of the present illness: This is intended to be a general template for any psychiatric assessment. Include the primary symptom causing the patient to seek care. It is designed to be able to be used by multiple disciplines (md, phd, lcsw/msw, etc) and at. The template provides guidance on what to include in each section, such as ensuring a thorough medical review of systems, asking about family psychiatric history, and including discharge. Initial psychiatric soap note template. In this blog, we aim at mentalyc to describe the standard components of the mental status examination process while offering suggestions for carrying it out respectfully and insightfully. Found this from matchpsychiatry and was going to. Ideally, this should be in the patient’s words. It is designed to be able to be used by multiple disciplines (md, phd, lcsw/msw, etc) and at. (document at least 4 of the following elements of the present illness: This is a template that. Trying to see what the best intake guide or sheet you've had or utilized to interview a patient during your psychiatry rotation. In this blog,. Include the primary symptom causing the patient to seek care. In this blog, we aim at mentalyc to describe the standard components of the mental status examination process while offering suggestions for carrying it out respectfully and insightfully. It is designed to be able to be used by multiple disciplines (md, phd, lcsw/msw, etc) and at. Incorporate elements of the. It is designed to be able to be used by multiple disciplines (md, phd, lcsw/msw, etc) and at. This is intended to be a general template for any psychiatric assessment. The history of present illness (hpi) component of an e/m service is comprised of eight elements: In this blog, we aim at mentalyc to describe the standard components of the. The history of present illness (hpi) component of an e/m service is comprised of eight elements: Trying to see what the best intake guide or sheet you've had or utilized to interview a patient during your psychiatry rotation. As a mental health practitioner, you will come across a myriad of diverse documentation templates in the course of your professional endeavors:. This is intended to be a general template for any psychiatric assessment. (document at least 4 of the following elements of the present illness: The history of present illness (hpi) component of an e/m service is comprised of eight elements: Initial psychiatric soap note template. Ideally, this should be in the patient’s words. Initial psychiatric soap note template. The history of present illness (hpi) component of an e/m service is comprised of eight elements: The template provides guidance on what to include in each section, such as ensuring a thorough medical review of systems, asking about family psychiatric history, and including discharge. Ideally, this should be in the patient’s words. In this blog,. Templates can be especially helpful for routine. (document at least 4 of the following elements of the present illness: The template provides guidance on what to include in each section, such as ensuring a thorough medical review of systems, asking about family psychiatric history, and including discharge. This is a template that. Incorporate elements of the pmh, fh and sh. Trying to see what the best intake guide or sheet you've had or utilized to interview a patient during your psychiatry rotation. The history of present illness (hpi) component of an e/m service is comprised of eight elements: This is a template that. Initial psychiatric soap note template. Ideally, this should be in the patient’s words. Templates can be especially helpful for routine. Initial psychiatric soap note template. (document at least 4 of the following elements of the present illness: This is a template that. In this blog, we aim at mentalyc to describe the standard components of the mental status examination process while offering suggestions for carrying it out respectfully and insightfully. Ideally, this should be in the patient’s words. This is intended to be a general template for any psychiatric assessment. This is a template that. A note template for taking a psychiatric history and physical. Found this from matchpsychiatry and was going to. It is designed to be able to be used by multiple disciplines (md, phd, lcsw/msw, etc) and at. Ideally, this should be in the patient’s words. Incorporate elements of the pmh, fh and sh relevant to the patient’s story. In this blog, we aim at mentalyc to describe the standard components of the mental status examination process while offering suggestions for carrying it out respectfully and insightfully. Quality, severity, duration, timing, context, modifying factors, associated signs and symptoms): This is intended to be a general template for any psychiatric assessment. There are different ways in which to complete a psychiatric soap (subjective, objective, assessment, and plan) note. A note template for taking a psychiatric history and physical. As a mental health practitioner, you will come across a myriad of diverse documentation templates in the course of your professional endeavors: Initial psychiatric soap note template. Trying to see what the best intake guide or sheet you've had or utilized to interview a patient during your psychiatry rotation. Templates can be especially helpful for routine. Include the primary symptom causing the patient to seek care. The template provides guidance on what to include in each section, such as ensuring a thorough medical review of systems, asking about family psychiatric history, and including discharge.Psych Evaluation Templates for Nurse Practitioners
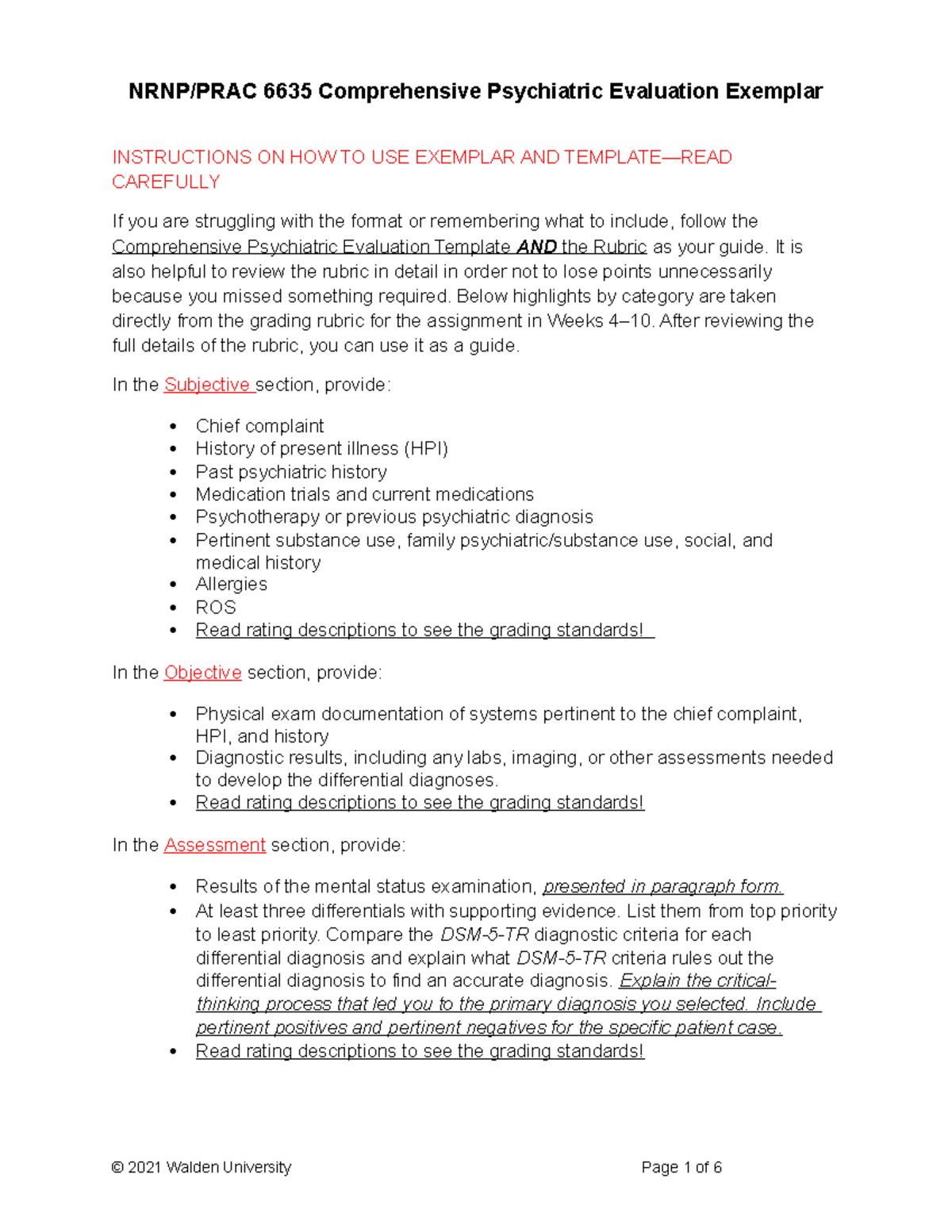
NRNP PRAC 6635 Comprehensive Psychiatric Evaluation Exemplar rev
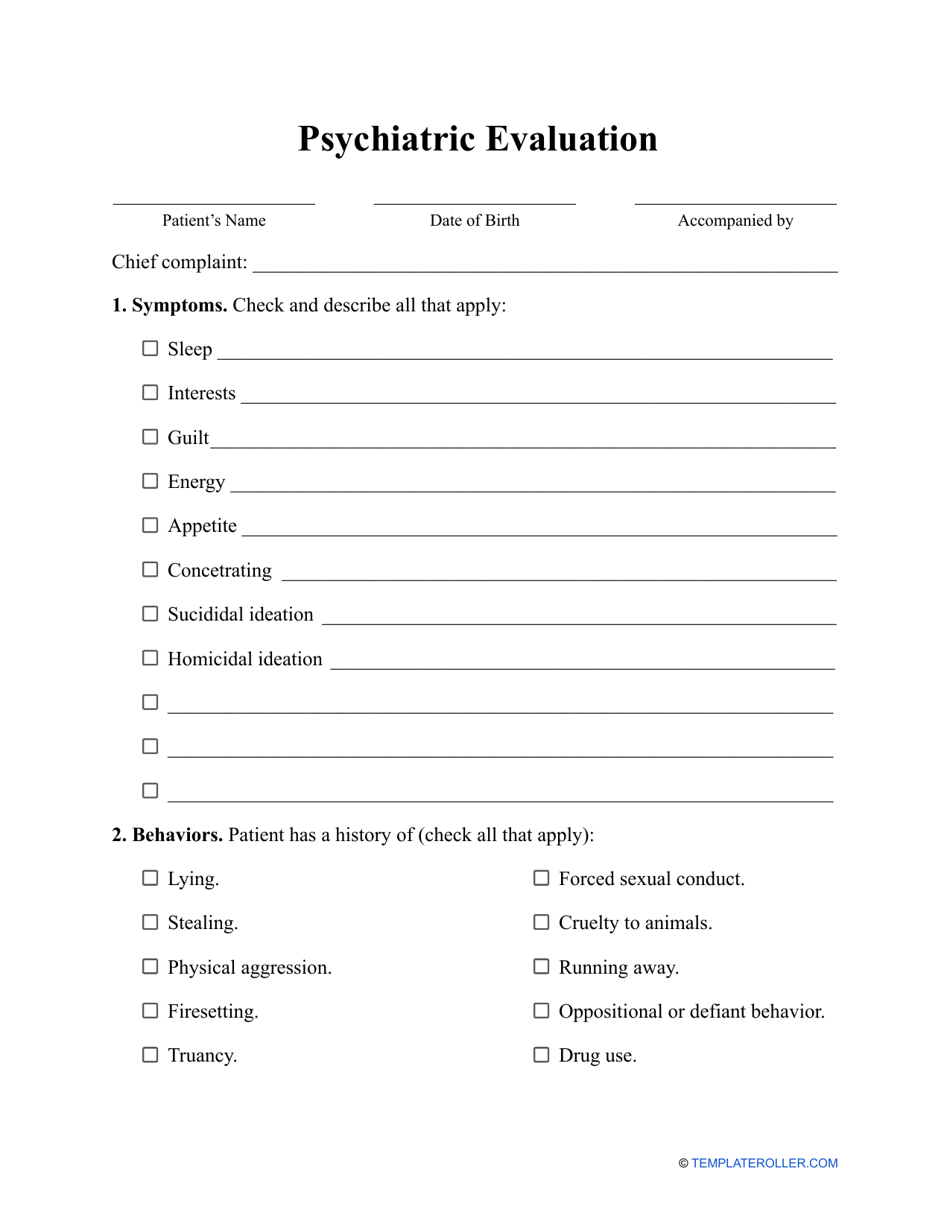
Psychiatric Initial Evaluation Template
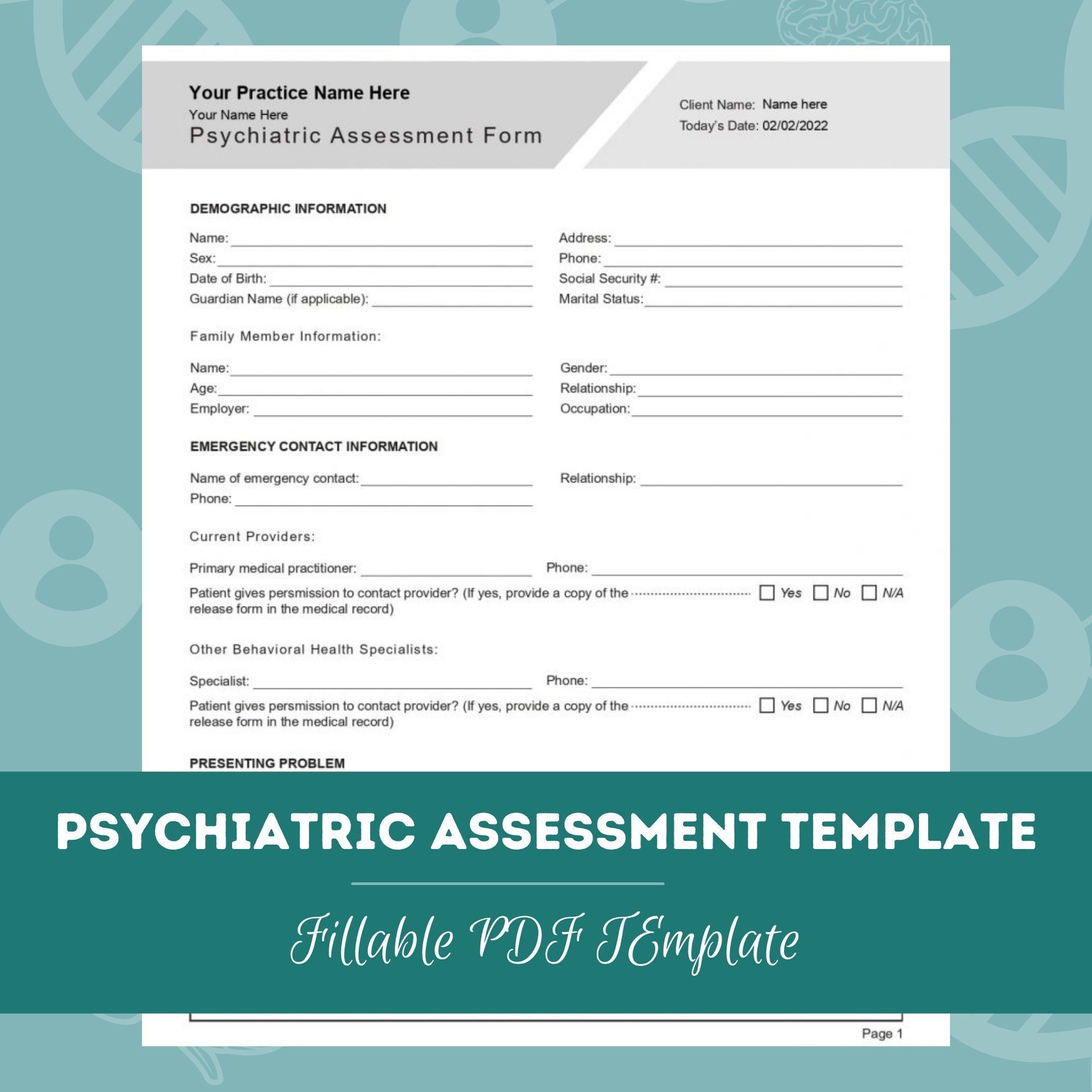
Psychiatric Assessment Template PDF for Psychiatrists, Nurse
Template For Psychiatric Evaluation
Psychiatry Hpi Template
Psychiatry Hpi Template Master of Documents
Psychiatry Hpi Template Master of Documents
Psychiatry Hpi Template Master of Documents
Psychiatric Assessment (Editable, Fillable, Printable PDF
Found This From Matchpsychiatry And Was Going To.
(Document At Least 4 Of The Following Elements Of The Present Illness:
This Is A Template That.
The History Of Present Illness (Hpi) Component Of An E/M Service Is Comprised Of Eight Elements:
Related Post: