Psych History Template
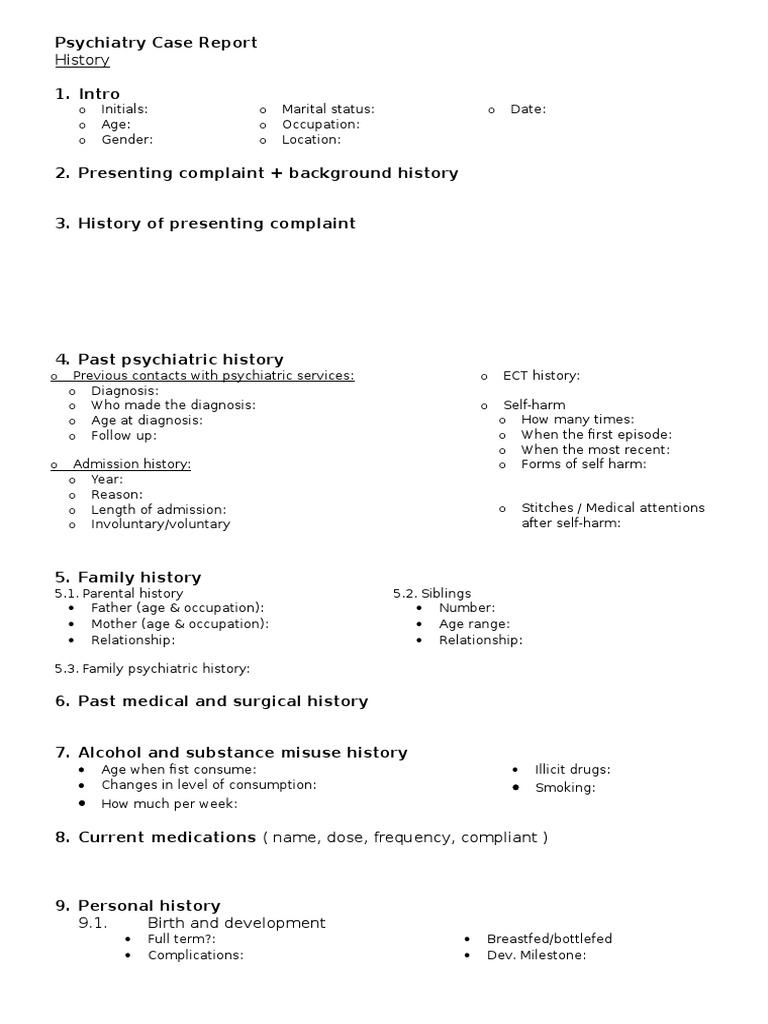
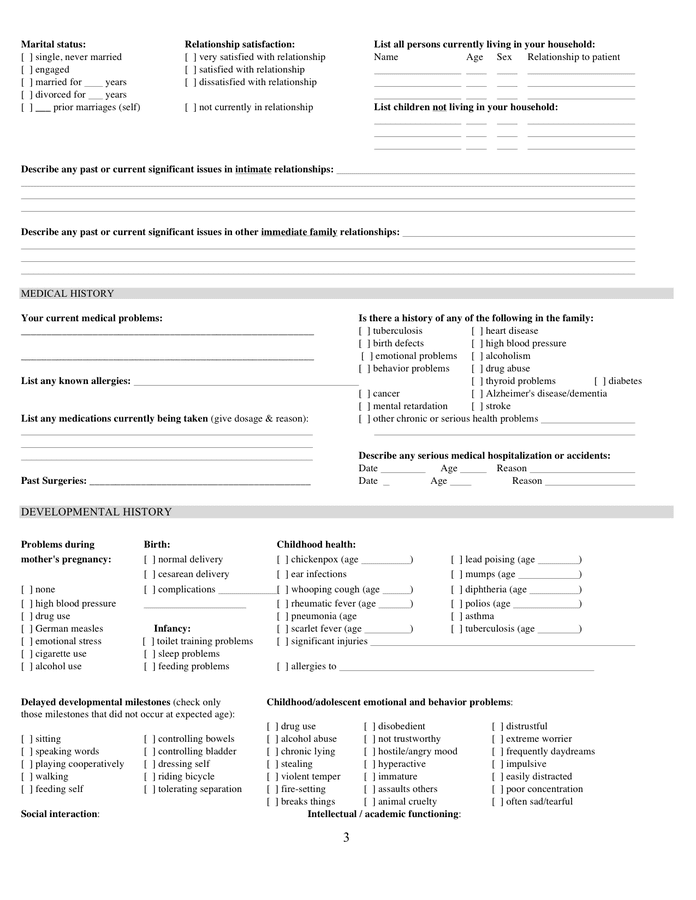
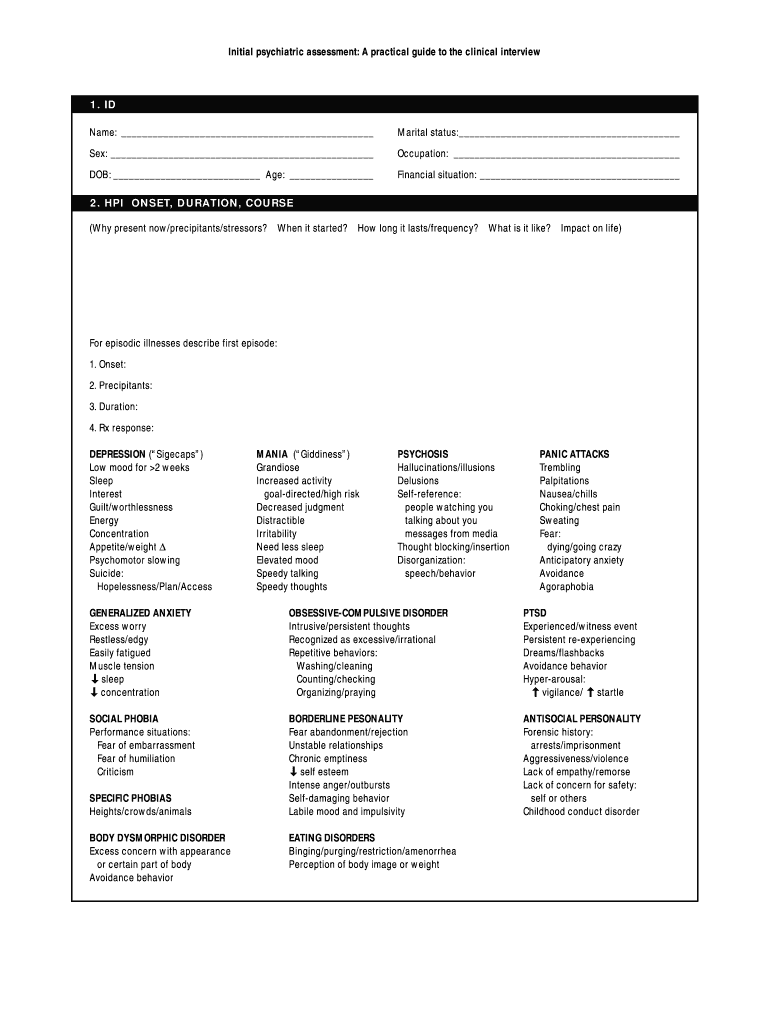
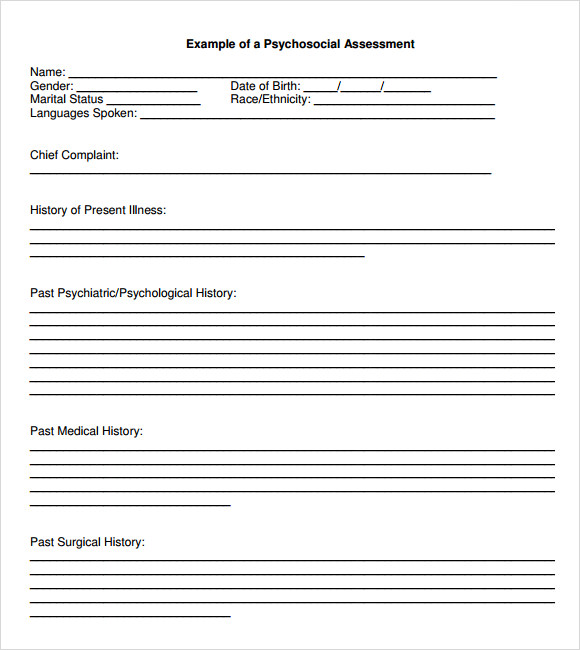
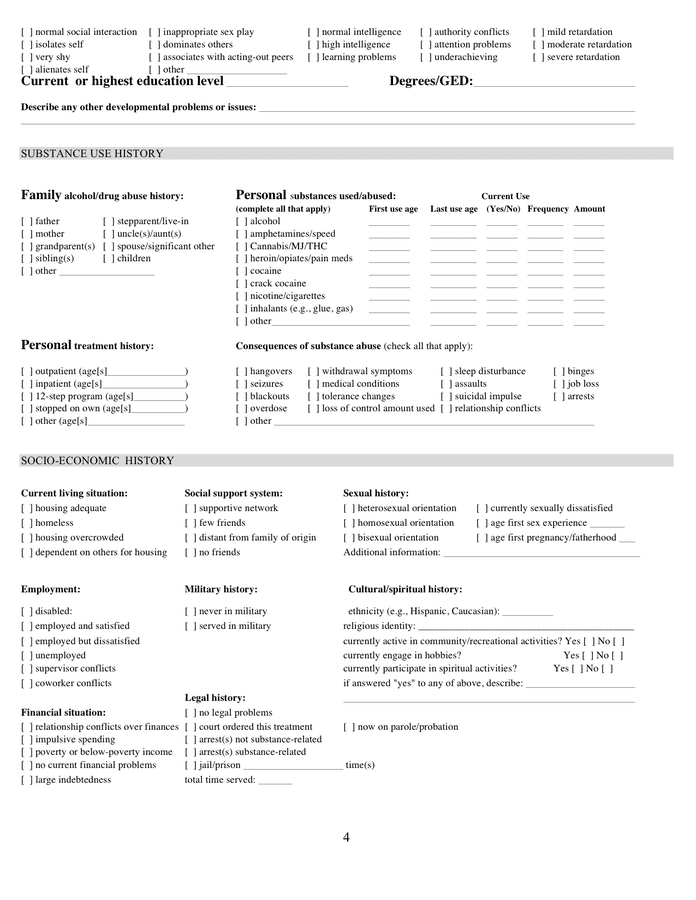
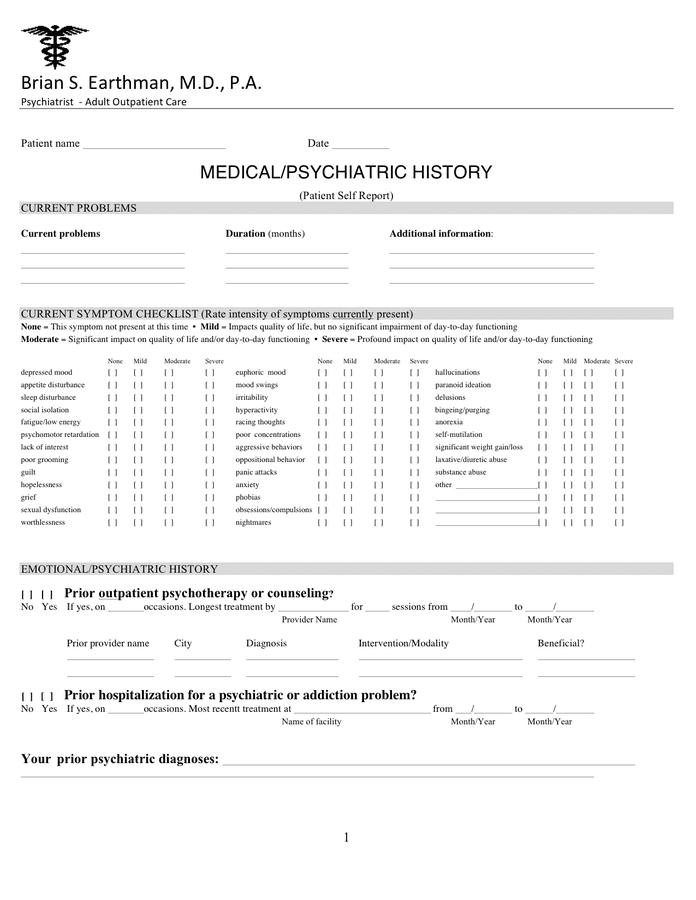
Psych History Template - Past psychiatric history 13 ask the patient about their past psychiatric history 14 establish past psychiatric diagnoses, treatments and past contact with mental health This document outlines a psychiatric history taking format that includes: Psychiatry progress note templates to streamline your practice. It also has an excellent diagnostic formulation. Hasnyone a in your family been diagnosed with or treated for any of the following (circle): Psychiatric hx previous psychiatric hx/counseling/suicide attempts/violence: Taking a depression history is an important skill that is often assessed in osces. This guide provides a structured approach to taking a depression history in an osce setting. Please list past psychiatric treatment providers, both outpatient and inpatient, as well as any substance abuse counseling or treatments. One of the most widely used formats for evaluation in psychology, psychiatry, and related domains is the mental status examination (mse). One of the most widely used formats for evaluation in psychology, psychiatry, and related domains is the mental status examination (mse). All levels of psych assessment. Past psychiatric history 13 ask the patient about their past psychiatric history 14 establish past psychiatric diagnoses, treatments and past contact with mental health Psychiatric hx previous psychiatric hx/counseling/suicide attempts/violence: A practical guide to the clinical interview 3. Depression history taking opening the consultation 1 wash your hands and don ppe if appropriate 2 introduce yourself to the patient including your name and role 3. Taking a depression history is an important skill that is often assessed in osces. Bipolar disorder anger alcohol abuse This guide provides a structured approach to taking a depression history in an osce setting. This document outlines a psychiatric history taking format that includes: State not provided here if not available. Taking a depression history is an important skill that is often assessed in osces. This document outlines a psychiatric history taking format that includes: Bipolar disorder anger alcohol abuse Conducting a mental status examination. Please list past psychiatric treatment providers, both outpatient and inpatient, as well as any substance abuse counseling or treatments. All levels of psych assessment. One of the most widely used formats for evaluation in psychology, psychiatry, and related domains is the mental status examination (mse). A practical guide to the clinical interview 3. Bipolar disorder anger alcohol abuse Psychiatric hx previous psychiatric hx/counseling/suicide attempts/violence: Psychiatry progress note templates to streamline your practice. Conducting a mental status examination. Depression history taking opening the consultation 1 wash your hands and don ppe if appropriate 2 introduce yourself to the patient including your name and role 3. Taking a depression history is an important skill that is often assessed in osces. Past psychiatric history 13 ask the patient about their past psychiatric history 14 establish past psychiatric diagnoses, treatments and past contact with mental health Identifying information about the patient and details of their chief complaint and history of present illness. It also has an excellent diagnostic formulation. Depression history taking opening the consultation 1 wash your hands and don ppe. It also has an excellent diagnostic formulation. Bipolar disorder anger alcohol abuse Reading this model case history, one will have an excellent understanding of the patient’s history, development, current situation and presentation. Conducting a mental status examination. Hasnyone a in your family been diagnosed with or treated for any of the following (circle): Click here for a guide and a free template copy! Past psychiatric history 13 ask the patient about their past psychiatric history 14 establish past psychiatric diagnoses, treatments and past contact with mental health State not provided here if not available. Depression history taking opening the consultation 1 wash your hands and don ppe if appropriate 2 introduce yourself to. Male include vital signs if provided. Please list past psychiatric treatment providers, both outpatient and inpatient, as well as any substance abuse counseling or treatments. It also has an excellent diagnostic formulation. A practical guide to the clinical interview 3. Reading this model case history, one will have an excellent understanding of the patient’s history, development, current situation and presentation. For psychiatrists, nurse practitioners, nurses, physician assistants, residents, and students. Identifying information about the patient and details of their chief complaint and history of present illness. This guide provides a structured approach to taking a depression history in an osce setting. Taking a depression history is an important skill that is often assessed in osces. Please list past psychiatric treatment. It also has an excellent diagnostic formulation. Psychiatry progress note templates to streamline your practice. Conducting a mental status examination. Taking a depression history is an important skill that is often assessed in osces. Past psychiatric history 13 ask the patient about their past psychiatric history 14 establish past psychiatric diagnoses, treatments and past contact with mental health It also has an excellent diagnostic formulation. This document outlines a psychiatric history taking format that includes: Depression history taking opening the consultation 1 wash your hands and don ppe if appropriate 2 introduce yourself to the patient including your name and role 3. Diagnose mental health problems and disorders with the help of our psychiatric evaluation template. All levels. Psychiatric hx previous psychiatric hx/counseling/suicide attempts/violence: Depression history taking opening the consultation 1 wash your hands and don ppe if appropriate 2 introduce yourself to the patient including your name and role 3. Diagnose mental health problems and disorders with the help of our psychiatric evaluation template. Reading this model case history, one will have an excellent understanding of the patient’s history, development, current situation and presentation. It also has an excellent diagnostic formulation. Identifying information about the patient and details of their chief complaint and history of present illness. State not provided here if not available. This document outlines a psychiatric history taking format that includes: A practical guide to the clinical interview 3. Psychiatry progress note templates to streamline your practice. Taking a depression history is an important skill that is often assessed in osces. All levels of psych assessment. Male include vital signs if provided. Hasnyone a in your family been diagnosed with or treated for any of the following (circle): Click here for a guide and a free template copy! Past psychiatric history 13 ask the patient about their past psychiatric history 14 establish past psychiatric diagnoses, treatments and past contact with mental healthPsychiatry Case Report template
Psychiatric History Template
Psychiatric Assessment (Editable, Fillable, Printable PDF
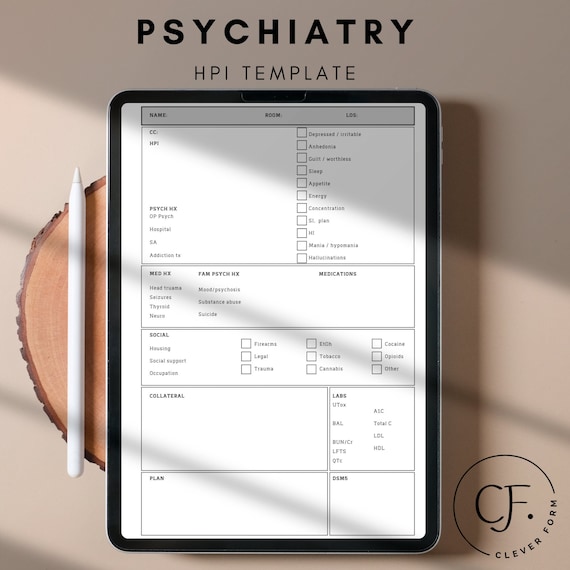
Psychiatry HPI template psych history and physical Etsy France
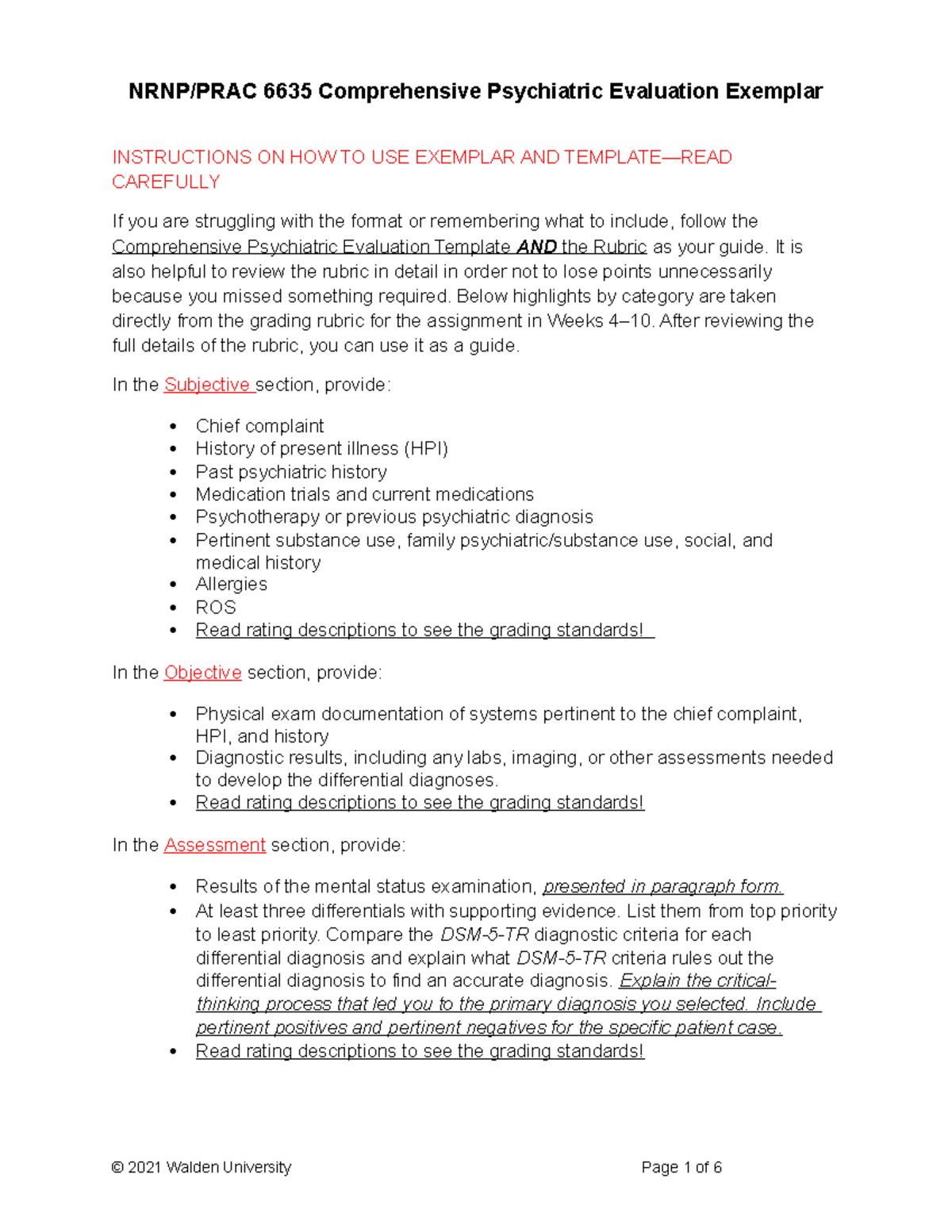
NRNP PRAC 6635 Comprehensive Psychiatric Evaluation Exemplar rev
Psychiatric Assessment Guide Fill Online, Printable, Fillable, Blank
St Joseph Psychiatric Hospital Orange County Psychiatric Assessment
NR 548 psychiatric history assignment Filled) Psychiatric History
Psychiatric History Template
Psychiatric History Template
Conducting A Mental Status Examination.
One Of The Most Widely Used Formats For Evaluation In Psychology, Psychiatry, And Related Domains Is The Mental Status Examination (Mse).
This Guide Provides A Structured Approach To Taking A Depression History In An Osce Setting.
For Psychiatrists, Nurse Practitioners, Nurses, Physician Assistants, Residents, And Students.
Related Post: