History And Physical Exam Template
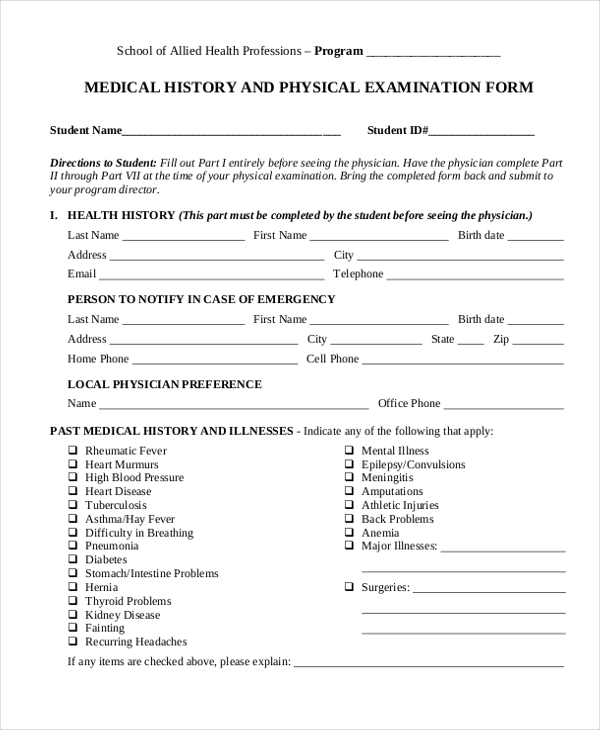
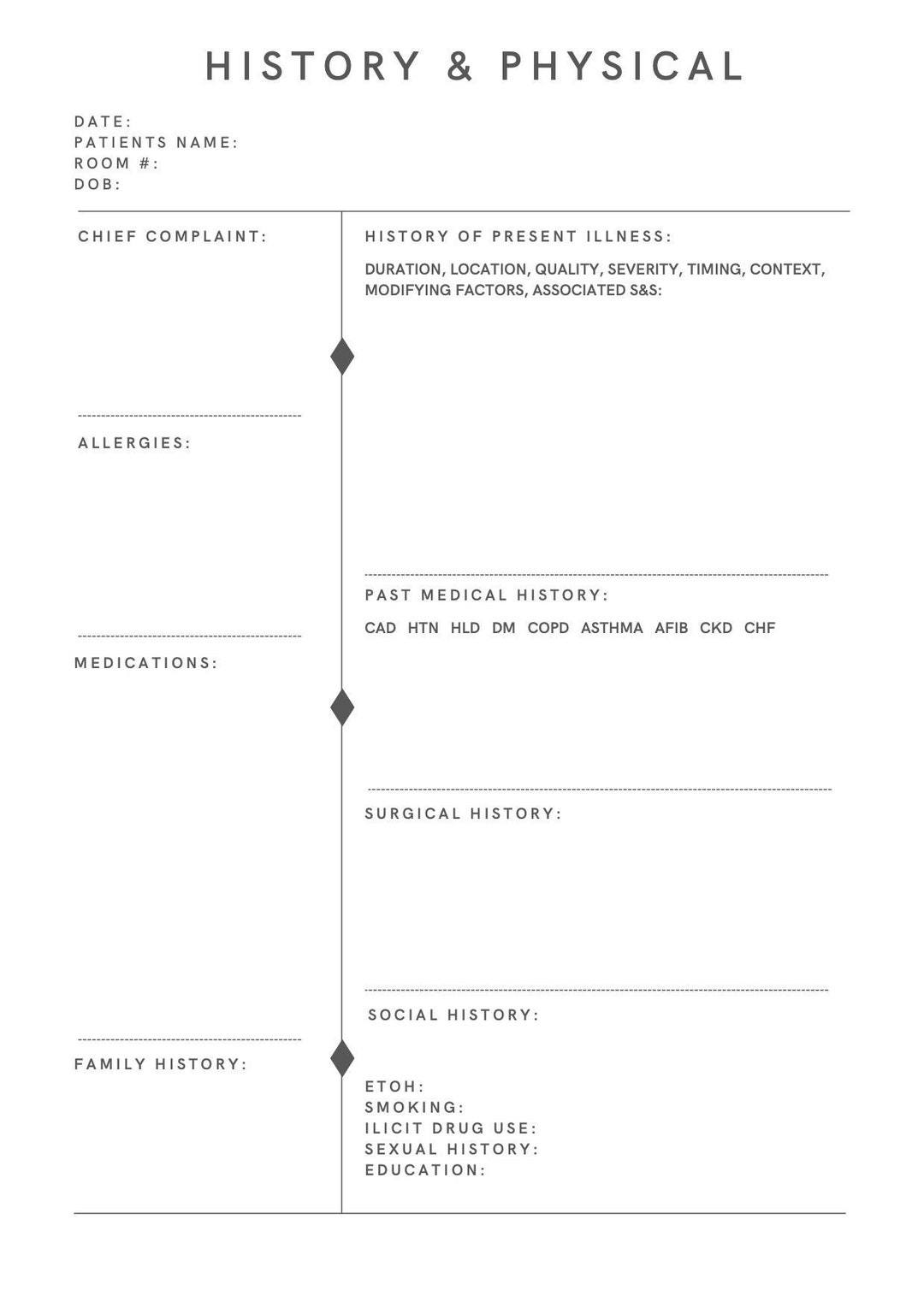
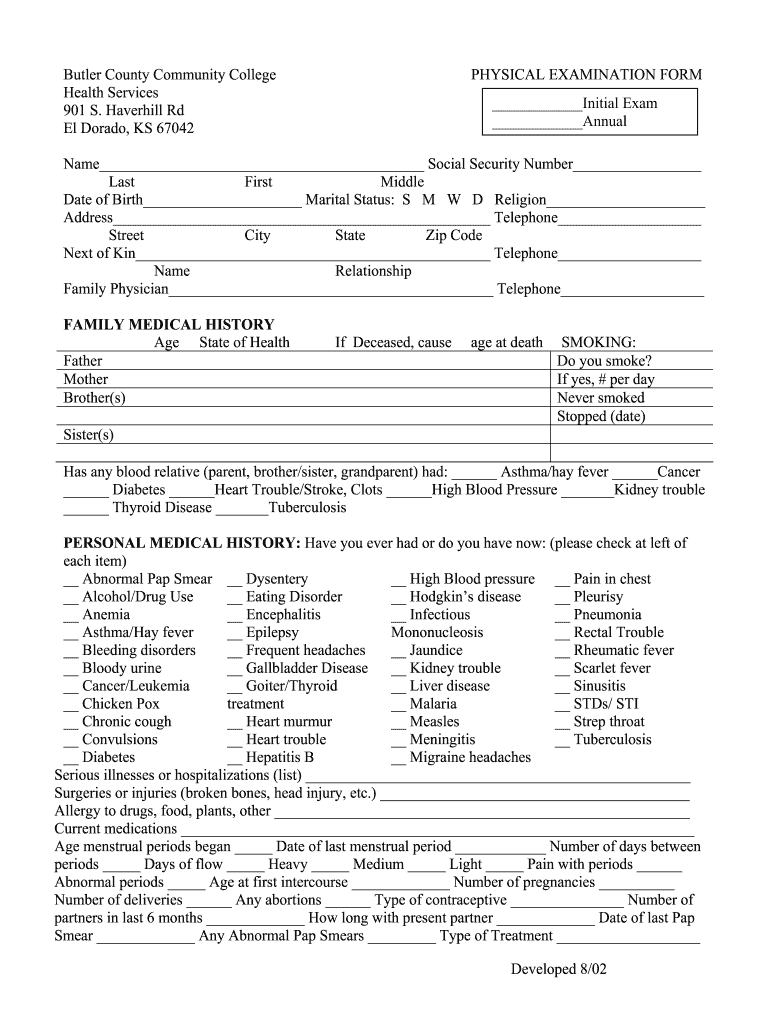
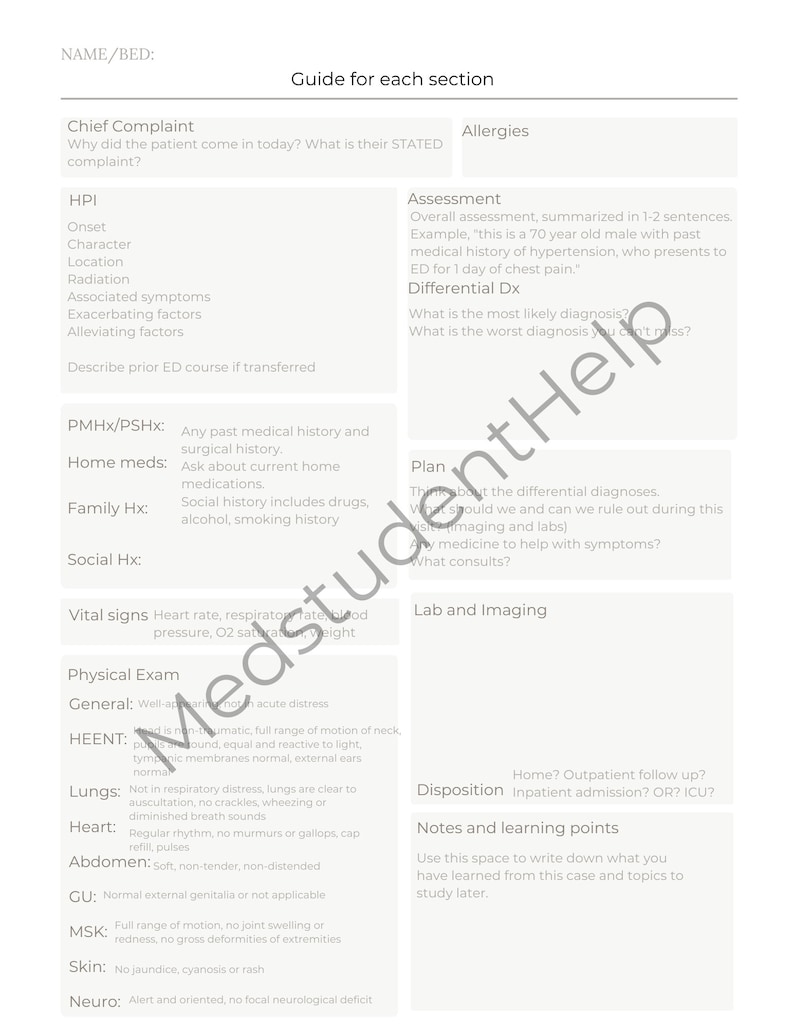
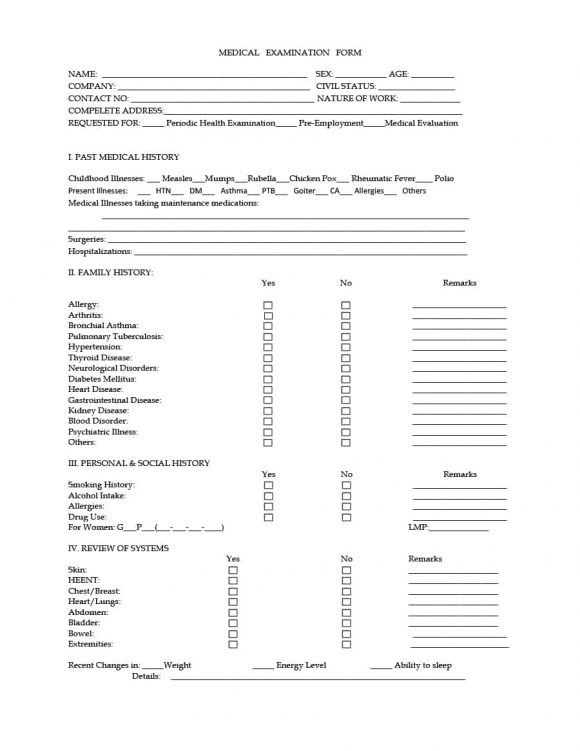
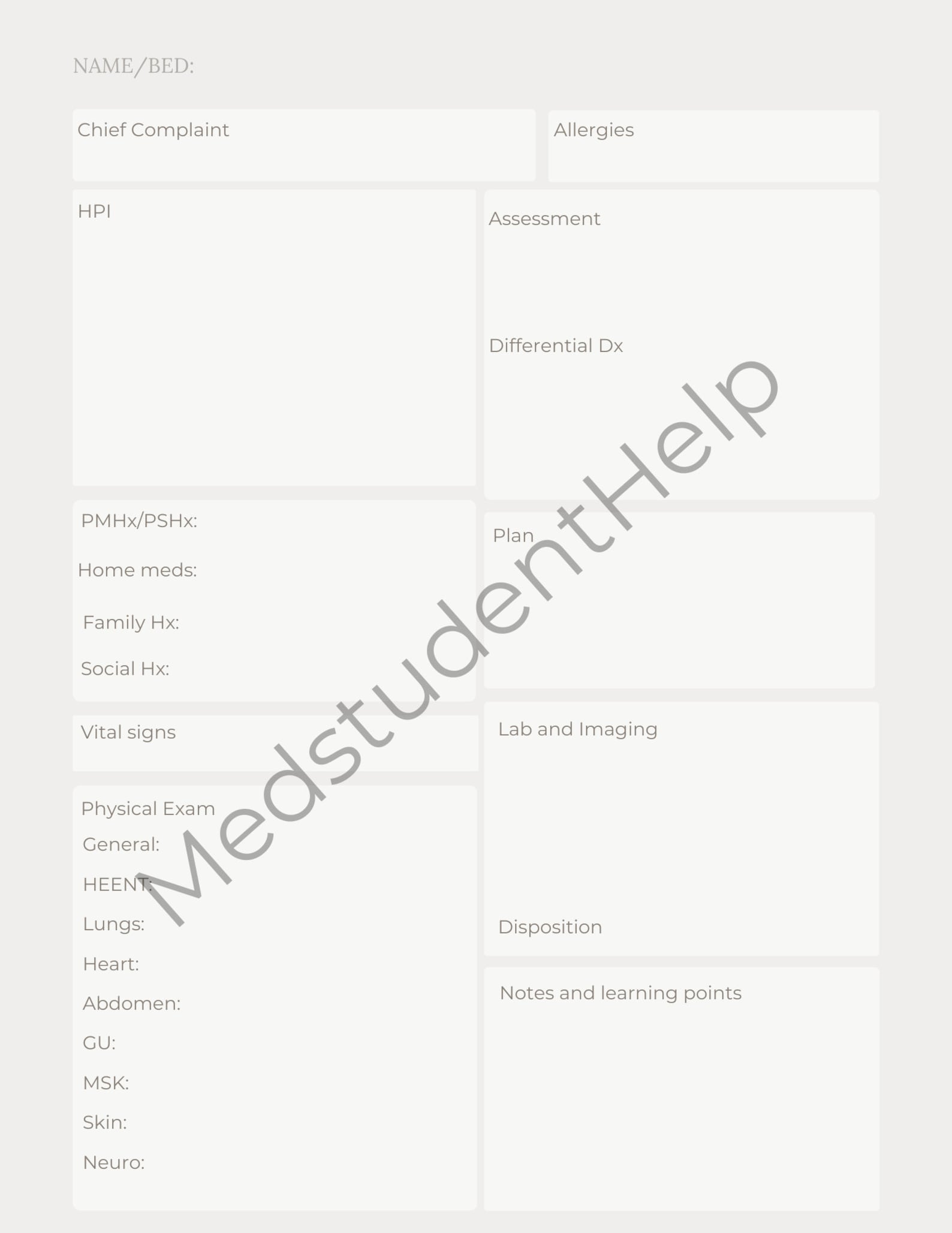
History And Physical Exam Template - The documentation template includes the following sections: Up to $50 cash back history and physical (h&p) template is a set of standardized forms and questions used by medical providers to document the medical history and physical. History and physical template cc: Verify insurance requirements for documentation to avoid billing issues later. This simple template contains the headings for a classic history and physical examination report. This document contains a patient intake form collecting demographic information, chief complaint, history of present illness, review of systems, past medical history, social history, vital signs,. View, change, and fill in history and physical form quickly at formspal! Include patient history and previous exam notes for a comprehensive view. Is an 83 year old retired nurse with a long history of hypertension that was previously well controlled on diuretic therapy. This document provides templates for taking a. This medical document contains sections for a patient's. Verify insurance requirements for documentation to avoid billing issues later. She was first admitted to. “i got lightheadedness and felt too weak to walk” source and setting: _____ social history (please check the appropriate listings) tobacco use alcohol use drug use The health history of a patient provides direction for their care and helps clarify the patient’s needs. Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: Include patient history and previous exam notes for a comprehensive view. It outlines the key sections to include such as the chief complaint, history of present illness,. Please comment on all positive findings and be sure all information is complete. A succinct description of the symptom (s) or situation responsible for the patient's presentation for health care. Chief complaint, history of present illness, review of systems, sexual assault, annual screening questionnaire,. Please review the patient’s history and complete the medical examination form. U or iu, trailing zeros (1.0) or leading zeros (.1), ms or mso4, mgso4, da or dop, db,. View, change, and fill in history and physical form quickly at formspal! History and physical template cc: She was first admitted to. A focused health history and a. Please comment on all positive findings and be sure all information is complete. This document provides a template for writing a history and physical examination report. Please review the patient’s history and complete the medical examination form. Verify insurance requirements for documentation to avoid billing issues later. U or iu, trailing zeros (1.0) or leading zeros (.1), ms or mso4, mgso4, da or dop, db, or. Chief complaint, history of present illness, review. There are two main nursing assessments: Chief complaint, history of present illness, review of systems, sexual assault, annual screening questionnaire,. A simple online service to download legal templates and pdfs in minutes. This medical document contains sections for a patient's. Include patient history and previous exam notes for a comprehensive view. This simple template contains the headings for a classic history and physical examination report. This medical document contains sections for a patient's. Please review the patient’s history and complete the medical examination form. The health history of a patient provides direction for their care and helps clarify the patient’s needs. _____ social history (please check the appropriate listings) tobacco use. Clerks and residents on our surgical team are encouraged to use it or a similar system. History and physical template cc: Comprehensive adult history and physical (sample summative h&p by m2 student) chief complaint: This medical document contains sections for a patient's. It outlines the key sections to include such as the chief complaint, history of present illness,. Please comment on all positive findings and be sure all information is complete. Include patient history and previous exam notes for a comprehensive view. U or iu, trailing zeros (1.0) or leading zeros (.1), ms or mso4, mgso4, da or dop, db, or. A succinct description of the symptom (s) or situation responsible for the patient's presentation for health care.. It is often helpful to use the. A succinct description of the symptom (s) or situation responsible for the patient's presentation for health care. History and physical template cc: Please review the patient’s history and complete the medical examination form. View, change, and fill in history and physical form quickly at formspal! This medical document contains sections for a patient's. The health history of a patient provides direction for their care and helps clarify the patient’s needs. Clerks and residents on our surgical team are encouraged to use it or a similar system. A focused health history and a. A simple online service to download legal templates and pdfs in minutes. It is often helpful to use the. “i got lightheadedness and felt too weak to walk” source and setting: There are two main nursing assessments: Please comment on all positive findings and be sure all information is complete. This document provides a template for writing a history and physical examination report. Past / family / social history (must include all 3) past medical / surgical hx/chronic medical. “i got lightheadedness and felt too weak to walk” source and setting: This simple template contains the headings for a classic history and physical examination report. The documentation template includes the following sections: _____ social history (please check the appropriate listings) tobacco use alcohol use drug use Up to $50 cash back history and physical (h&p) template is a set of standardized forms and questions used by medical providers to document the medical history and physical. Include patient history and previous exam notes for a comprehensive view. This document contains a patient intake form collecting demographic information, chief complaint, history of present illness, review of systems, past medical history, social history, vital signs,. A succinct description of the symptom (s) or situation responsible for the patient's presentation for health care. Please review the patient’s history and complete the medical examination form. She was first admitted to. Chief complaint, history of present illness, review of systems, sexual assault, annual screening questionnaire,. View, change, and fill in history and physical form quickly at formspal! It is often helpful to use the. Please comment on all positive findings and be sure all information is complete. This document provides templates for taking a.Printable History and Physical Exam Template Etsy
History And Physical Template
History & Physical Exam
History and Physical Template, Nurse Practitioner Student, Nursing
College Physical Form Fill Online, Printable, Fillable, Blank pdfFiller
Printable History and Physical Exam Template Etsy
Classical medical history And Physical examination template. in 2020
Physician History And Physical Template Master of Documents
Printable History and Physical Exam Template Etsy
Free Printable Basic Physical Exam Form Pdf
This Document Provides A Template For Writing A History And Physical Examination Report.
A Focused Health History And A.
A Simple Online Service To Download Legal Templates And Pdfs In Minutes.
U Or Iu, Trailing Zeros (1.0) Or Leading Zeros (.1), Ms Or Mso4, Mgso4, Da Or Dop, Db, Or.
Related Post: